Management of Epidural Analgesia
Management of Epidural Analgesia
Course Description
This course discusses various aspects of epidural analgesia including procedures, complications, pharmacological properties and patient assessment.
Accreditation Information: KLA Education Services LLC is accredited by the State of California Board of Registered Nursing, Provider # CEP16145.
Course Certification: Once you have completed this course, click on the “Print Certificate” option below to save or print your CE course certification. If you are not yet registered in a course plan with IvyLeagueNurse, please complete the registration and payment process so that you are able to log into your account and fully obtain your course certificate. Our affordable and unlimited one-year CEU plan starts at just $19.99.
Print Certificate Print Course
Course Objectives
Upon completion of this course, the course participant will be able to:
- Three anatomical relevance to complications expressed in epidural analgesia
- Two unique physiological expression in epidural block different from systemic pain medication administration
- Two surgical procedures appropriately supported by the epidural analgesia administered into the thoracic space
- Two irreversible complications associated with epidural analgesia
- Three categories of pharmacological agents administered via epidural catheter
- Two pharmacological properties of each of the three drug classes utilized in epidural analgesia
- The procedure for the determination of sensory block
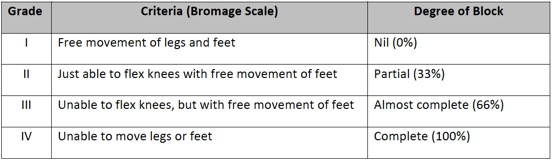
- The method for assessing the extent of the motor block
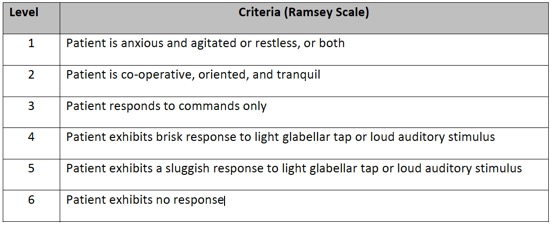
- The scale for assessing the level of consciousness
- Two factors determining patient’s ability to ambulate
- The timing for catheter removal if patient is on pharmacological deep vein thrombosis (DVT) prophylaxis
Course Content
Introduction
Epidural analgesia is a regional method effective for intraoperative anesthetic augmentation and post operative pain management. The range of application includes labor and delivery and thoracic, abdominal, gynecological, urological, orthopedic, and vascular procedures. Drugs administered to the epidural space potently block the first synaptic nociceptive signal transmission from the spinal cord to the periphery. Small doses of pharmaceutical agents directly applied to the nerve roots elicit strong analgesia, particularly when a combination therapy of narcotics and local anesthetics is employed for the synergic effects. The adverse side effects of drowsiness, confusion, constipation, urinary retention, itchiness, nausea and respiratory depression of epidural analgesia are greatly reduced compared to those of systemically generated by higher doses of oral or intravenous preparations. However, the epidural route of administration is not without its potential risks. The timely and proper assessment of the patient receiving analgesia via epidural catheter is essential for the prevention of rare, but serious complications ranging from inadequate pain control to irreversible neurological sequelae caused by hematoma or abscess formation within the epidural space.
PRECAUTIONS/KEY POINTS
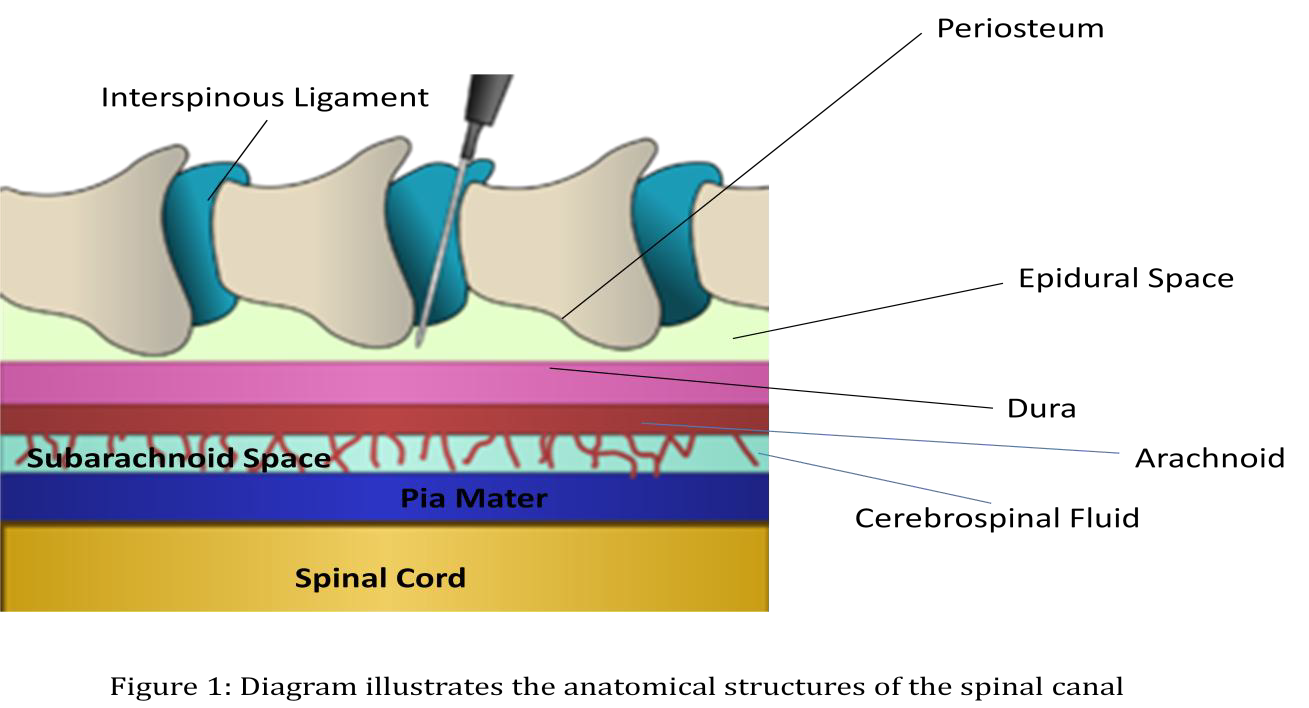
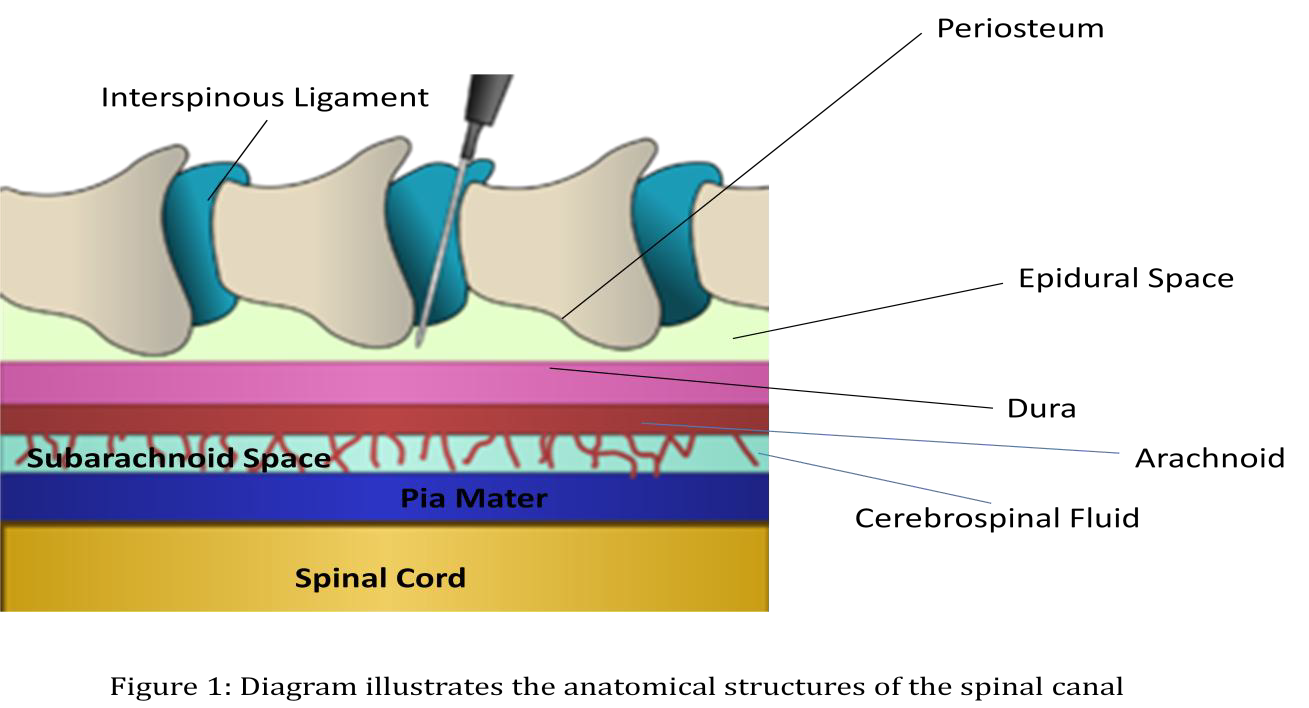
Understanding the anatomy and physiology of the epidural space and its related structures (Figure 1) is fundamentally important for the recognition of mechanisms of epidural blockade and potential complications.
-
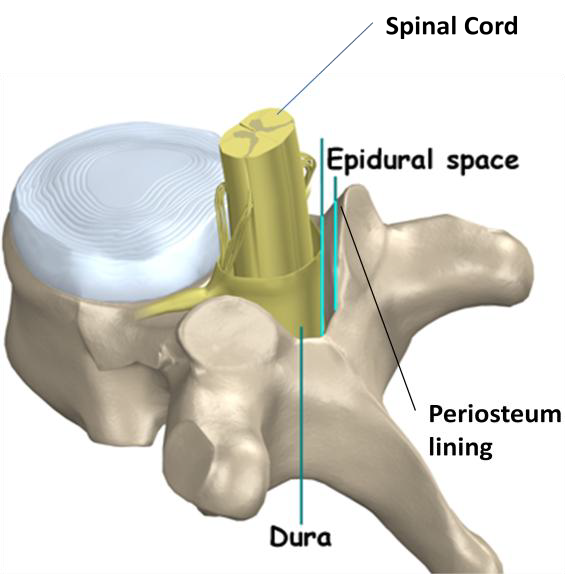
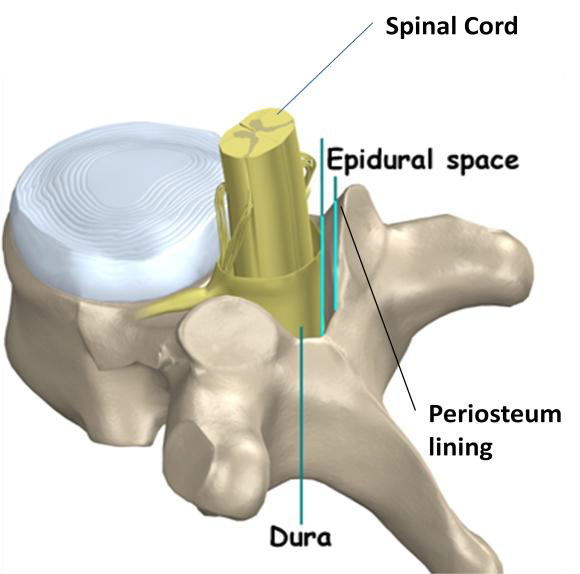
The epidural space is a potential space which lies within the spinal canal between the external dural membrane and the periosteum lining of the vertebral structure. This space along the canal is anatomically butting against the bony vertebral structures (Figure 2) and thereby limited to volume expansion. Any dramatic size increase due to hematoma or abscess formation in this space will cause severe impingement of the nerve roots and spinal cord. If immediate surgical decompression is not rendered, paralysis will become the debilitating lifelong consequence.
-
The epidural space is richly embedded with venous plexuses and adipose tissues. Patients exhibiting coagulopathy or receiving anticoagulant therapy are contraindicated for epidural analgesia. The potential for bleeding during catheter placement is amplified with the above conditions. The post operative deep vein thrombosis prophylaxis and removal of epidural catheter requires meticulous attention to timing for dosing and choice of appropriate anticoagulant therapy.
-
Epidural analgesia is contraindicated for a patient with unexplained neurological symptoms, active neurological disease, localized infection in lumbar area, systemic sepsis or bleeding disorders.
-
Within the epidural space, the converging nerve fibers conduct outgoing and incoming signal transmissions to mediate the survival instincts and functionality of the human body. The small myelinated sympathetic fibers which control the “fight or flight” responses are most susceptible to pharmacological blockade while the large motor fibers are least sensitive to drug actions. Therefore, the neuraxial blockade is clinically manifested in the descending sequence of sympathetic, sensory and motor capability loss. Medications can be adjusted in concentration and volume to provide regional block without compromising the motor control and hemodynamic regulation. Epidural agents such as fentanyl and local anesthetics can further impact the sympathetic nerve fibers triggering intense hypotension and alarming bradycardia.
-
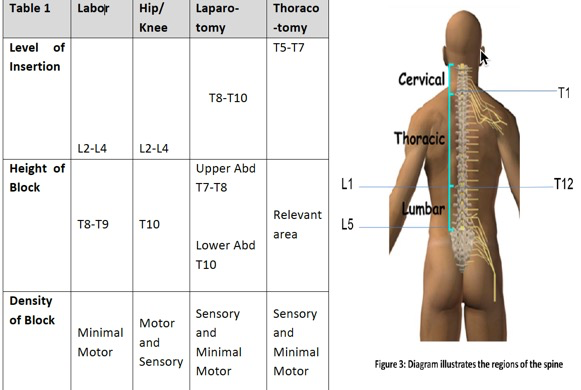
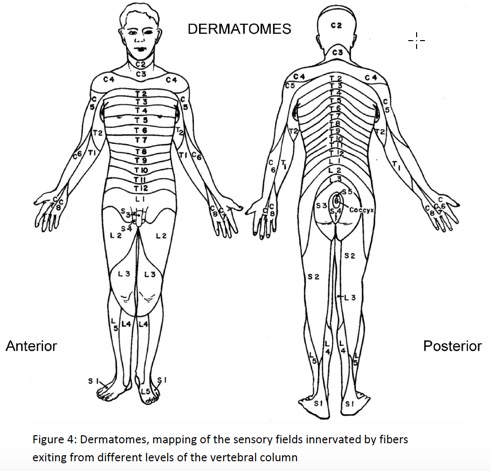
The epidural catheter is anatomically inserted at a level appropriate to the site of surgery (Table 1). The extent of the sensory blockade expressed in dermatomes will vary depending upon the site of catheter insertion (i.e. lumbar, abdominal, thoracic) and the density of agents determined by the volume and concentration of drugs administered. An agent of a more diluted concentration but administered at a higher volume can exert a high level of block with less adverse side effects.

-
Dermatomes (Figure 4) are the mapping of sensory expression innervated by the corresponding sensory nerve fibers from different segments of the spine. The loss of sensation two to three levels above the catheter tip placement provides adequate post operative pain control, whereas beyond the normal levels of sensory blockade reflects inadvertently high block. Epidural analgesia administered above the lumbar region exerts regional effects with minimal effect over the motor ability. For the patient post abdominal surgery or thoracotomy receiving epidural analgesia, ambulation should be an integral part of the plan of care. The accurate assessment of sensory and motor block and vital signs is important to determine adequate pain control and ambulating ability, and furthermore, to recognize hemodynamic instability.
-
The spinal cord terminates at the L2 level in adult. Thus, the potential for injury to the spinal cord is greatly reduced when the epidural catheter insertion site is at or below L2.
PHARMACOLOGY OF EPIDURAL ANALGESIA
1. Pharmacologic agents commonly used for epidural analgesia include local anesthetics, opioids, or alpha agonists which can be used alone or in combination.
a. Local anesthetics-Bupivacaine (Marcaine), chloroprocaine, or lidocaine (Xylocaine)
b. Opioids-Morphine, duramorph (preservative free morphine), fentanyl (a synthetic opioid which is 100 times more potent than morphine) or sufentanil (shorter acting, but 5 to 10 times more potent than fentanyl). The hydrophilic opioid (such as morphine) is desirable for single dose injection which sustains pain control for a long duration from (12 to 18 hours) without motor impairment.
c. Alpha agonists-Clonidine or epinephrine can be used as an adjuvant to augment the analgesic effect of the local anesthetics and prolong its duration of actions. The alpha agonist is generally used as a substitute for the opioid in combination therapy to avoid unwanted side effects from narcotics.
2. The pathways of drug absorption/distribution within the epidural space include:
a. Diffusion through the dura into the various spinal structures/components
b. Uptake by vasculature within the epidural space
c. Absorption by fatty tissues in the epidural space serving as a depository for slow release
3. Local anesthetic toxicities can be extensive if considerable amounts of drug enter the epidural vasculature. They include light-headedness, tinnitus, circumoral tingling and numbness, anxiety, confusion, tremor, convulsion, coma and cardio-pulmonary arrest. If toxicities are suspected, stop epidural infusion and provide supportive measures until the toxic drug effects dissipate.
4. Opioid induced respiratory depression and over-sedation can be reversed by narcan.
5. Modes of epidural analgesia administration
a. Single shot injection
b. Intermittent boluses
c. Continuous infusion
d. Continuous infusion with intermittent boluses for breakthrough pain
POTENTIAL COMPLICATIONS
1. Hypotension is a rather common side effect because the sympathetic fibers are most sensitive to the agents used in epidural analgesia. It is also more likely associated with blockade above the umbilicus and epidural administration without incremental dosing.
2. Other common adverse side effects are excessive sensory loss above the norm of 2 to 3 levels, unintended motor block, urinary retention, pruritus, inadequate pain control, nausea, vomiting, confusion, disorientation, and drowsiness.
3. Serious/life-threatening complications include paresthesia, cerebrospinal fluid leak, respiratory depression, epidural hematoma or abscess, and paralysis. Although rare, inadvertent total spinal block can happen.
4. Catheter insertion site infection is usually associated with back pain, tenderness, erythema, swelling, drainage, and fever.
5. Dural puncture/Post dural headache is uncommon in caudal epidural placement since the spinal cord terminates at the space between L1 and L2 in adult. The headache will be alleviated with bed rest, adequate hydration and mild analgesics as needed. Unfortunately, these measures will serve only as supportive measures, not a cure. In severe cases, an epidural blood patch may be required to seal the leakage.
6. Inadvertent high epidural block can occur when large doses of local anesthetic accumulate in the epidural space. The intercostal muscles may be paralyzed and intubation will become necessary for life-support.
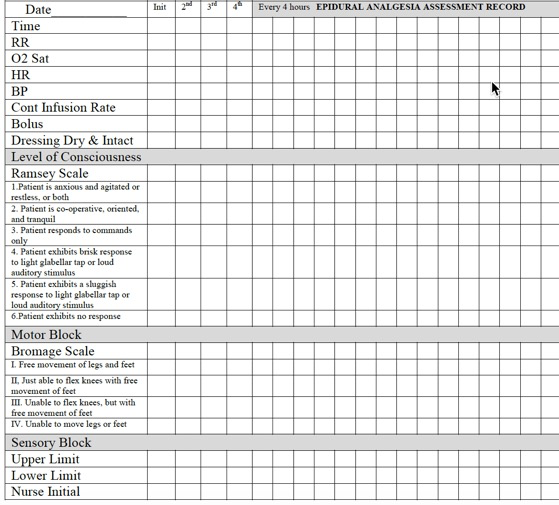
ASSESSMENT
1. On arrival from the Post Anesthesia Care Unit (PACU) or Operating Room (OR), inspect the epidural insertion site to ensure proper securement of the catheter (Figure 5), and the clear window dressing being dry (i.e. no leakage of cerebrospinal fluid), without tenderness, redness or swelling, clean and intact. The catheter is customarily taped to the shoulder and attached with a 0.2 micron filter/adaptor for intermittent boluses or continuous infusion. The injection port should be clearly labeled with the sign of “For Epidural Injection Only”.
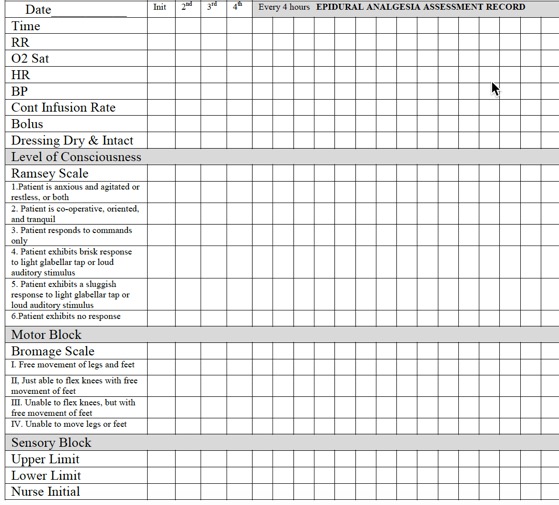
2. Assessment frequency is hourly for the first four hours from arrival to the admitting unit, then every four hours thereafter if stable. Continue assessment for 24 hours after the last bolus dose before the removal of epidural catheter.
3. Assessment criteria include the following:
a. Epidural catheter insertion site
b. Vitals: Temperature, pulse/rhythms, blood pressure, respiration rate and continuous oxygen saturation
c. Pain level assessed with the 0-10 numeric pain intensity rating scale
d. Level of consciousness assessed with Ramsey Scale
e. Motor block is assessed with Bromage Scale-Ambulate patient only if assessed with Grade I or Grade II.
f. Sensory block is assessed with the following procedure:
i. Explain procedure to the patient
ii. Wrap ice with a 4x4 gauze
iii. Apply wrapped ice to the forehead and ask patient to tell you how cold the ice feels
iv. Place wrapped ice to a location likely to be blocked bilaterally and at approximately the same level as the epidural catheter insertion site. Ask the patient if he/she feels the same degree of coldness as the forehead or different temperature. Patients may report the ice feeling colder, warmer, or the same.
v. Apply the ice above and below until it is clear about the upper and lower limit of the sensory block.
vi. Repeat the above step on the opposite side.
g. Inform Anesthesia with abnormal findings
SUMMARY
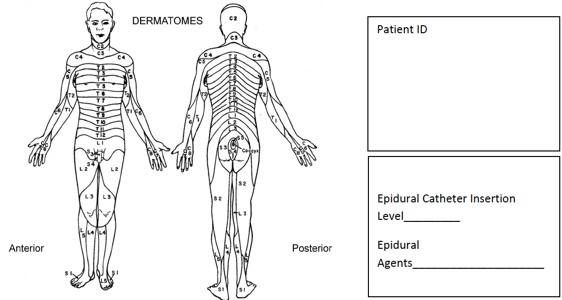
During the early development of caudal analgesia in the 1940s, this procedure was employed as a disparate measure for the survival of the recipient. In modern medicine, the application of epidural analgesia in labor and delivery and post operative pain management is becoming increasingly popular over the last half century. The benefits of epidural analgesia have been demonstrated in effectiveness and efficacy with greatly reduced rates of systemic side effects, stress induced myocardial infarction and impaired mobility. However, the safety of the patient receiving epidural analgesia is determined by the knowledge and technical competency (Attachment 1: Assessment Record is attached for your learning) possessed by the nurse managing his/her care.
REFERENCES
Bird, A., & Wallis, M. (2002). Nursing knowledge and assessment skills in the management of patients receiving analgesia via epidural infusion. Journal of Advanced Nursing, 40(5), 522-531.
Donatelli, F., Tran, D., Mistraletti, G., & Carli, F. (2005). Epidural analgesia in the Post-Anesthesia Care Unit. Current Drug Targetts, 6, 795-806.
Hader, C. F. (2007). Epidural analgesia in the critically ill. Nursing 2007 Critical Care, 2(5).
Rodgers, A., Walker,N., Schug, S. et al. (2000). Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomized trials. British Medical Journal, 321,1493-7.
Ueda,K., Ueda, W., Manabe, M. (2005). A comparative study of sequential epidural bolus technique and continuous epidural infusion. Anesthesiology. 103(1): 126-9.
Walsh, K. (2010). Pain, Postoperative: Epidural analgesia. Cinahl Information Systems.
Weetman, C., & Allison, W. (2006, July 12). Use of epidural analgesia in post-operative pain management. Nursing Standard, 20(44), 54-64.
ATTACHMENTS
Attachment 1
Attachment 2

Course Exam
Before you receive your certificate, you must complete the exam and achieve a score of % or higher. (You have unlimted attempts).
This exam is required by your state licensure.
Exam
Exam
We are required to delay the exam hours. Check back soon!
Exam
We are required to delay the exam until you have had time to view the course material. Please view the course first!
No Licenses on File
Please add a license to your account before you continue. Thank you!