Infection Prevention and Control in Long Term Care Part 1
Infection Prevention and Control in Long Term Care Part 1
Course Description
Infection Prevention and Control in Long Term Care is discussed including risks for bloodbourne infections, PPE, hand washing, biohazardous waste, and biological terrorism pathogens.
Accreditation Information: KLA Education Services LLC is accredited by the State of California Board of Registered Nursing, Provider # CEP16145.
Course Certification: Once you have completed this course, click on the “Print Certificate” option below to save or print your CE course certification. If you are not yet registered in a course plan with IvyLeagueNurse, please complete the registration and payment process so that you are able to log into your account and fully obtain your course certificate. Our affordable and unlimited one-year CEU plan starts at just $19.99.
Print Certificate Print Course
Course Objectives
Upon completion of this course, the course participant will be able to:
- List 5 risks for bloodbourne infection
- Describe PPE
- Describe proper hand washing
- List 3 types of biohazardous waste
- List 4 types of biological terrorism pathogens
Course Content
Purpose
-
Adhere to the overall infection prevention and control programs as required by the CMS (§483.65) and the OSHA Bloodborne Pathogen Standard (29CFR 1910.1030)
-
Introduce current standards of practice identified through the guidance of the CDC specific to long term care
-
Implement new/improved skills in the management of infection prevention and control
-
Improve the quality of care
Why?
-
F441 is one of the top 5 deficiencies cited across the United States
-
McGeer’s criteria for surveillance definitions were revised in 2012 (1st revision since 1991)
-
National increase in MDRO’s – specifically C. Difficile
-
Recognized knowledge gap in understanding the requirements of an effective infection and control program in long term care
The Regulation
§483.65 (F441) “The facility must establish and maintain an infection control program designed to provide a safe, sanitary, and comfortable environment and to help prevent the development and transmission of diseases and infection.”
AND...
“The facility must establish an infection control program under which it:
- Investigates, control and prevents infections in the facility;
- Decides what procedures, such as isolation should be applied to an individual resident;
- Maintains a record of incidents and corrective actions related to infections.”
AND...
-
“When the infection control program determines that a resident needs isolation to prevent the spread of infection, the facility must isolate the resident.”
-
“The facility must prohibit employees with a communicable disease or infected skin lesions from direct contact with residents or their food, if direct contract will transmit the disease.”
-
“The facility must require staff to wash their hands after each direct resident contact for which hand washing is indicated by accepted professional practice.”
-
“Personnel must handle, store, process and transport linens so as to prevent the spread of infection.”
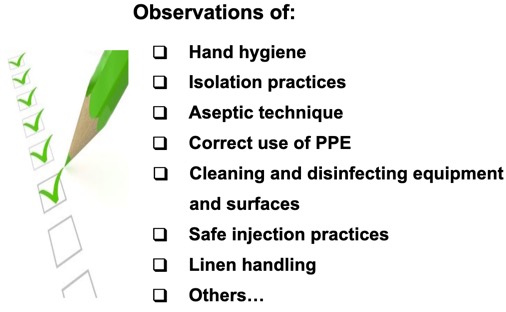
Components of IPC Program

Surveyor Review
Blood Pathogens & Needlestick Prevention
OSHA
-
Bloodborne Pathogen Regulation - CFR 1910.130
-
Determination of employee exposure
- Work practices and control measures
-
Education, training and employee responsibility
-
Hepatitis B vaccinations
-
Post exposure to bloodborne pathogens
-
Employee health records, confidentiality and availability
-
Bloodborne Pathogen
-
Infectious conditions that reach their target area through the circulation of blood
-
Disease is transmitted from one person’s blood to another’s
-
Produce acute and chronic infections
-
Bloodborne pathogens of greatest concern:
-
Human immunodeficiency virus (HIV)
-
Hepatitis B virus (HBV)
-
Hepatitis C virus (HCV)
-
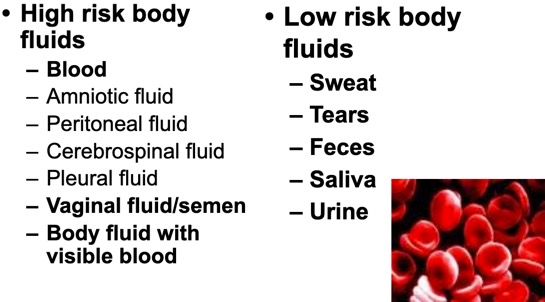
Risk Exposure Activities
Activities/situations where employees may incur occupational exposure to blood or other potentially infectious materials without regards to the use of PPE.
Risk of BBP Infection
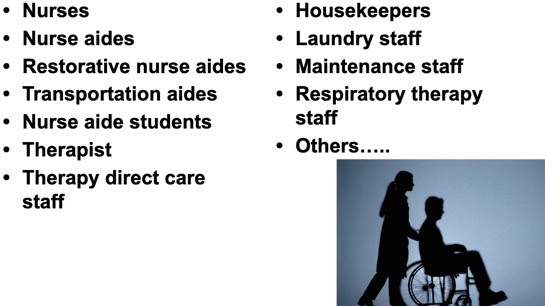
Job Classifications at Risk
Risk of BBP Disease
-
HIV
-
Needlestick: 0.3%
-
Splash: less than 0.3%
-
-
Hepatitis B
-
Needlestick: up to 30%
-
-
Hepatitis C
-
Needlestick: up to 10%
-
(2009 APIC)
Work Practice Control Measures
-
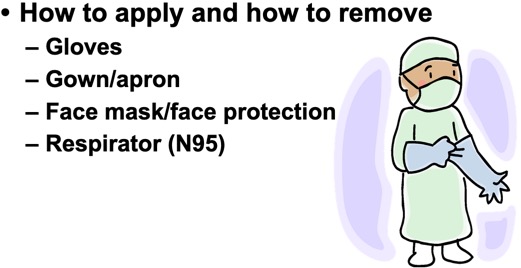
Personal protective equipment
-
Standard precautions & hand hygiene
-
Safe injection practices
-
Biohazardous waste management
-
Blood spill management
-
Specimen management
-
Cleaning and disinfecting
-
Laundry management
-
Exposure management
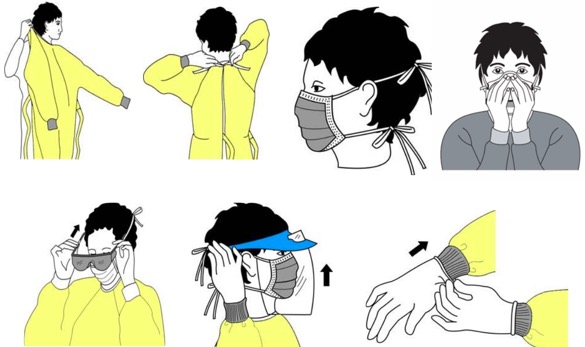
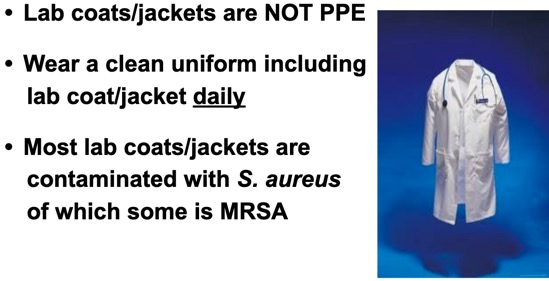
Personal Protective Equipment
Hand Hygiene
-
Hand washing with soap & water
-
Hand rubbing with alcohol based hand rub (ABHR)
Safe Injection Practices
-
The Needlestick Safety and Prevention Act (NSPA) went into affect April 18, 2001.
-
Intent of act is to reduce health care workers' exposure to BBP by imposing additional requirements upon employers concerning sharps procedures.
-
Needleless system devices used wherever possible and discarded following use in a sharps container.
-
Competency checks in use of devices
-
- No employee will bend, recap or break used syringe needles before discarding them into a sharps container.
- Exposed sharps will not be left on beds, bedside tables, or on work surfaces.
-
Sharps containers will be easily accessible to staff and located in areas where sharps are used.
-
Labeled and/or color coded as biohazard
-
Replace containers when ¾ full
-
DO NOT re-open closed container
-
Discard with biohazardous waste
-
NSPA
Consistent with the Act, OSHA's regulations
- (1) modify definition of "engineering controls" and adds definitions for terms "sharps with engineered sharps injury protection" and "needleless systems,“
- (2) requires employers to consider/implement new technologies when updating "exposure control plan,"
- (3) requires employers to solicit employee input for engineering controls, and
- (4) requires employers to maintain sharps injury log.
Examples of Sharps

Sharps Container
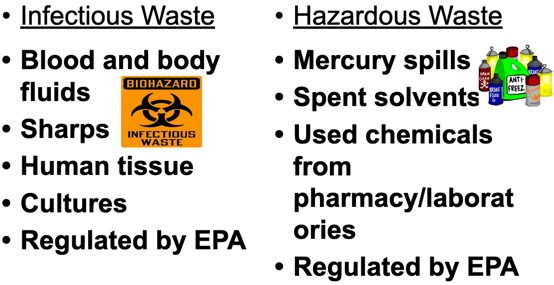
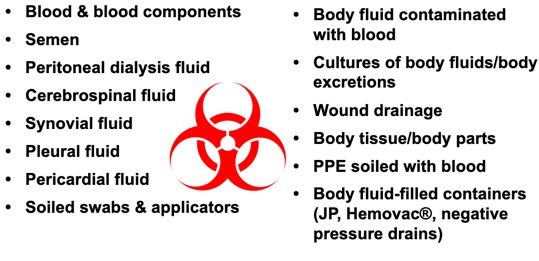
Biohazardous Waste
-
AKA regulated waste, infectious waste
-
Items that would release blood or other potentially infectious materials in a liquid or semi-liquid state if compressed
-
Items that are caked with dried blood or other potentially infectious materials capable of releasing these materials during handling. (OSHA)
-
Waste that contains pathogens with sufficient virulence and quantity so that exposure to the waste by a susceptible host could result in an infectious disease. (EPA)
Waste Comparison
Examples of Biohazardous Waste
Red Bags
-
Plastic red bags used to collect biohazardous waste at the site of origin
-
Designated locked locations
-
Labeled
-
Removal by transport agency
-
Documentation
Blood Spills

Specimens, Housekeeping, Laundry
Education
Hepatitis

Hepatitis B Vaccinations
-
3 dose series
-
1st dose within 10 days of employment
-
2nd dose in 1 month after 1st dose
-
3rd dose approx. 5 months after 2nd dose
-
-
Provide the vaccine information sheet (VIS)
-
Serology testing (anti-BHs) 1 – 2 months after 3rd dose is received
BBP Diseases
Hepatitis
-
Can be HBV or HCV that leads to hepatitis
-
Incubation: up to 3 months after exposure
-
Attacks liver cells
-
Signs/Symptoms: flu-like illness, N & V, jaundice, dark urine, clay-colored stool
HIV
-
Leads to AIDS
-
Conversion from HIV to AIDS can take years
-
Attacks immune system
-
Signs/Symptoms: frequent opportunistic infections, skin lesions, night sweats, cachexia
Hepatitis - Common Types
Hepatitis B
-
Virus attacks liver
-
Outcome: most adults have full recovery
-
10% develop chronic liver disease
-
S/S may not be present until 3 months after exposure
-
Preventable by vaccine!
Hepatitis C
-
Virus attacks liver
-
Outcome: 85% develop chronic HCV infection, cirrhosis & cancer
-
70% have no S/S
-
Up to 10 – 20 years before S/S present
-
No vaccine
HIV/AIDS
-
Viral infection of immune system
-
S/S: flu-like illness, period of asymptomatic, opportunistic infections
-
Outcome: No cure (currently), treatment available with antiviral drugs to prolong life
-
Prevention: No vaccine
Post Exposure Prophylaxis (PEP)
-
What is an exposure?
-
Infectious body fluid
-
Portal of entry
-
-
What is the risk?
-
Percutaneous ~ 1/300
-
Mucous membrane ~ 1/1000
-
Cutaneous ~ 1/1000
-
Exposure Incident
-
Report to supervisor immediately
-
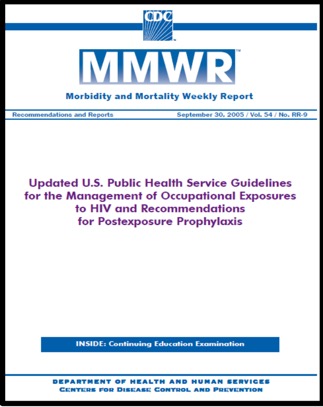
Follow guidance of the U.S. Public Health Service
-
Post exposure management
-
Time sensitive – hours vs. days
-
No cost to employee
-
Test source immediately
-
Offer counseling
-
-
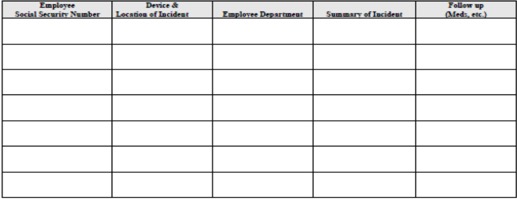
Sharps Injury Log (OSHA 300 Log)
-
Bloodborne Pathogen Exposure Report
-
Employee Consent to Blood Testing
-
Post-exposure Prophylaxis (PEP)
PEP Testing
-
Baseline blood testing
-
Source person
-
Exposed person
-
-
Follow-up blood testing
-
HIV 6, 12, 24 weeks
-
HBV none
-
HCV 6, 12, 24 weeks
-
Sharps Injury Log
Morbidity and Mortality Weekly Report
Employee Health Records
-
Confidential
-
Accessible to employee
-
Accessible to OSHA
-
Retained for duration of employment plus 30 years
Help with PEP
-
Free consultation for clinicians treating occupational exposures to HIV and other BBP
-
24/7 access
-
1-888-HIV-4911
-
Biological Terrorism
-
THE U.S. PUBLIC HEALTH SYSTEM AND PRIMARY HEALTHCARE PROVIDERS MUST BE PREPARED TO ADDRESS VARIOUS BIOLOGICAL AGENTS, INCLUDING PATHOGENS THAT ARE RARELY SEEN IN THE UNITED STATES. HIGH-PRIORITY AGENTS INCLUDE ORGANISMS THAT POSE A RISK TO NATIONAL SECURITY BECAUSE THEY
-
CAN BE EASILY DISSEMINATED OR TRANSMITTED FROM PERSON TO PERSON;
-
RESULT IN HIGH MORTALITY RATES AND HAVE THE POTENTIAL FOR MAJOR PUBLIC HEALTH IMPACT;
-
MIGHT CAUSE PUBLIC PANIC AND SOCIAL DISRUPTION;
-
REQUIRE SPECIAL ACTION FOR PUBLIC HEALTH PREPAREDNESS.
-
- AGENTS/DISEASES
-
Biological and Chemical Terrorism
Anthrax Spores

How Dangerous is Anthrax?
- CDC classifies agents with recognized bioterrorism potential into three priority categories. Anthrax is classified as a Category A agent, meaning those that:
-
Need a great deal of planning to protect the public’s health
-
Spread across a large area or need public awareness
-
Pose greatest possible threat for a bad effect on public health
-
-
Early treatment with ABT can cure cutaneous anthrax. Gastrointestinal anthrax is more serious with 1/4 to 1/2 of cases leading to death. Inhalation anthrax is more severe with up to 1/2 of the cases ending in death.
Anthrax Symptoms
-
SYMPTOMS OF ANTHRAX ARE DIFFERENT DEPENDING ON THE TYPE OF THE DISEASE:
-
CUTANEOUS: FIRST SYMPTOM IS A SMALL SORE THAT DEVELOPS INTO A BLISTER. THE BLISTER THEN DEVELOPS INTO A SKIN ULCER WITH A BLACK AREA IN THE CENTER. THE SORE, BLISTER AND ULCER DO NOT HURT.
-
GASTROINTESTINAL: FIRST SYMPTOMS ARE NAUSEA, LOSS OF APPETITE, BLOODY DIARRHEA, AND FEVER, FOLLOWED BY BAD STOMACH PAIN.
-
INHALATION: FIRST SYMPTOMS ARE COLD/FLU LIKE AND INCLUDE A SORE THROAT, MILD FEVER AND MUSCLE ACHES. LATER SYMPTOMS INCLUDE COUGH, CHEST DISCOMFORT, SHORTNESS OF BREATH, TIREDNESS AND MUSCLE ACHES.
-
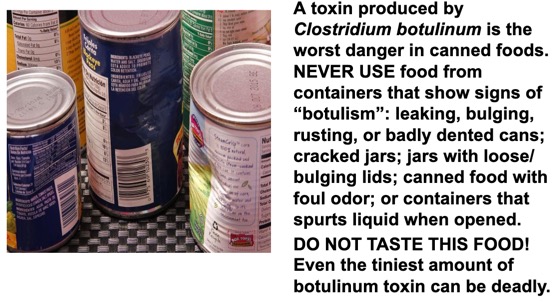
Botulism
FOODBORNE BOTULISM OCCURS WHEN A PERSON INGESTS PRE-FORMED TOXIN THAT LEADS TO ILLNESS WITHIN A FEW HOURS TO DAYS.
FOODBORNE BOTULISM IS A PUBLIC HEALTH EMERGENCY BECAUSE THE CONTAMINATED FOOD MAY STILL BE AVAILABLE TO OTHER PERSONS BESIDES THE PATIENT.
Botulism Symptoms
-
BEGIN WITHIN 6 HOURS UP TO 10 DAYS (MOST COMMONLY 12 - 36 HOURS) AFTER EATING FOOD THAT CONTAINS THE TOXIN.
-
INCLUDE DOUBLE VISION, BLURRED VISION, DROOPING EYELIDS, SLURRED SPEECH, DIFFICULTY SWALLOWING, DRY MOUTH, AND MUSCLE WEAKNESS THAT MOVES DOWN THE BODY, USUALLY AFFECTING THE SHOULDERS, THEN THE UPPER ARMS, LOWER ARMS, THIGHS, CALVES, ETC.
-
PARALYSIS OF BREATHING MUSCLES CAN CAUSE A PERSON TO STOP BREATHING AND DIE UNLESS MECHANICAL VENTILATION IS PROVIDED.
Botulism in Foods
Plague
-
WHY ARE WE CONCERNED ABOUT PNEUMONIC PLAGUE AS A BIOWEAPON?
-
YERSINIA PESTIS USED IN AN AEROSOL ATTACK COULD CAUSE CASES OF THE PNEUMONIC FORM OF PLAGUE. ONE TO SIX DAYS AFTER BECOMING INFECTED WITH THE BACTERIA, PEOPLE WOULD DEVELOP PNEUMONIC PLAGUE.
-
ONCE PEOPLE HAVE DISEASE, THE BACTERIA SPREADS TO OTHERS WHO HAVE CLOSE CONTACT.
-
BECAUSE OF THE DELAY BETWEEN BEING EXPOSED TO BACTERIA AND BECOMING SICK, PEOPLE COULD TRAVEL OVER A LARGE AREA BEFORE BECOMING CONTAGIOUS AND INFECTING OTHERS.
-
CONTROLLING THE DISEASE WOULD BE DIFFICULT.
-
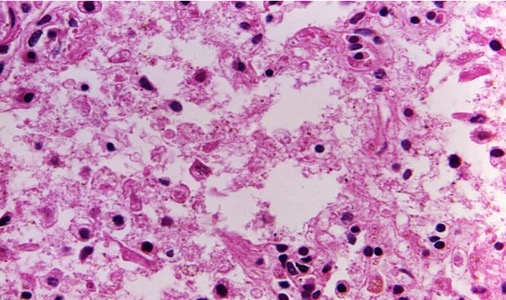
Pneumonic Plague
Plague Symptoms
-
WHAT ARE THE SIGNS AND SYMPTOMS OF PNEUMONIC PLAGUE?
-
FEVER, WEAKNESS, AND RAPIDLY DEVELOPING PNEUMONIA WITH SHORTNESS OF BREATH, CHEST PAIN, COUGH, AND SOMETIMES BLOODY OR WATERY SPUTUM.
-
-
-
NAUSEA, VOMITING, AND ABDOMINAL PAIN MAY ALSO OCCUR.
-
WITHOUT EARLY TREATMENT, PNEUMONIC PLAGUE USUALLY LEADS TO RESPIRATORY FAILURE, SHOCK, AND RAPID DEATH.
-
Smallpox

-
Although smallpox was declared globally eradicated in 1980, there is concern that smallpox virus may exist outside the two WHO-designated repository laboratories.
-
A single case of smallpox is likely to represent a bioterrorism release and will require an immediate and coordinated public health, medical, and law enforcement response to control the outbreak and to protect the public from any additional release.
-
Variola virus, an orthopoxvirus, is the etiological agent of smallpox. The only known reservoir for the virus is humans; there are no known animal or insect reservoirs or vectors.
-
Mode of transmission is person-to-person spread via direct deposit of infective droplets onto the nasal, oral, or pharyngeal mucosal membranes or in the alveoli of the lungs from close, face-to-face contact with an infectious individual.
-
Indirect spread via fine-particle aerosols or fomites has been reported but is less common.
Smallpox Symptoms
-
Initial S/S consists of high fever, malaise, severe headache and backache
-
This stage is followed by a maculopapular rash (eruptive stage) that progresses to papules (1 to 2 days after appearance of rash), vesicles (~ 4th to 5th day), pustules (by ~ 7th day), and finally scab lesions (~ 14th day)
-
Rash appears first on oral mucosa, face, & forearms & then spreads to trunk & legs
-
Skin lesions are deeply embedded in dermis and feel like firm, round objects under the skin
-
As lesions heal and scabs separate, pitted scarring develops
-
Overall mortality rate is approximately 30%
Chemical Terrorism
-
Bring all residents, visitors, families, staff indoors
-
Close all windows, air vents, dampers
-
Turn off fans, air conditioners and forced air heating systems
-
Seal all windows, doors and air vents
-
Shower immediately
-
If eyes are affected flush with saline
-
Follow instructions from local and/or state authorities
Bioterrorism Information
Course Description
Course Objectives
Course Content
- Purpose
- Why?
- The Regulation
- Components of IPC Program
- Surveyor Review
- Blood Pathogens & Needlestick Prevention
- Bloodborne Pathogen
- Risk Exposure Activities
- Risk of BBP Infection
- Job Classifications at Risk
- Risk of BBP Disease
- Work Practice Control Measures
- Personal Protective Equipment
- Hand Hygiene
- Safe Injection Practices
- NSPA
- Examples of Sharps
- Sharps Container
- Biohazardous Waste
- Waste Comparison
- Examples of Biohazardous Waste
- Red Bags
- Blood Spills
- Specimens, Housekeeping, Laundry
- Education
- Hepatitis
- Hepatitis B Vaccinations
- BBP Diseases
- Hepatitis - Common Types
- HIV/AIDS
- Post Exposure Prophylaxis (PEP)
- Exposure Incident
- PEP Testing
- Sharps Injury Log
- Morbidity and Mortality Weekly Report
- Employee Health Records
- Help with PEP
- Biological Terrorism
- Biological and Chemical Terrorism
- Anthrax Spores
- How Dangerous is Anthrax?
- Anthrax Symptoms
- Botulism
- Botulism Symptoms
- Botulism in Foods
- Plague
- Pneumonic Plague
- Plague Symptoms
- Smallpox
- Smallpox Symptoms
- Chemical Terrorism
- Bioterrorism Information
Course Exam
Before you receive your certificate, you must complete the exam and achieve a score of % or higher. (You have unlimted attempts).
This exam is required by your state licensure.
Exam
Exam
We are required to delay the exam hours. Check back soon!
Exam
We are required to delay the exam until you have had time to view the course material. Please view the course first!
No Licenses on File
Please add a license to your account before you continue. Thank you!
