Ultrasound Guided Peripheral IV Insertion
Ultrasound Guided Peripheral IV Insertion
Course Description
This course covers the use of ultrasound equipment to aid in peripheral IV insertion and includes content on items such as technology, vessel and catheter selection, site preparation, techniques, complications, and potential pitfalls.
Accreditation Information: KLA Education Services LLC is accredited by the State of California Board of Registered Nursing, Provider # CEP16145.
Course Certification: Once you have completed this course, click on the “Print Certificate” option below to save or print your CE course certification. If you are not yet registered in a course plan with IvyLeagueNurse, please complete the registration and payment process so that you are able to log into your account and fully obtain your course certificate. Our affordable and unlimited one-year CEU plan starts at just $19.99.
Print Certificate Print Course
Course Objectives
Upon completion of this course, the course participant will be able to:
- be able to describe human peripheral venous anatomy
- be familiar with the basics of high frequency-low depth ultrasound equipment
- be able to describe the vein/catheter selection process
- be able to demonstrate technique for cannulating a vessel using ultrasound
- be able to list 3 common pitfalls of learning this technique
- be able to list 3 potential complications of peripheral IV insertions
Course Content
In preparing for a successful ultrasound guided PIV start, there are several considerations to be made. These include: facility policy, ultrasound equipment, vessel and catheter selection, site preparation, technique for probe, insertion & threading, potential pitfalls & complications to avoid, and appropriate documentation.
Introduction
- Using ultrasound to insert peripheral intravenous catheters (PIVs) has been a common practice for years, however this skill is scarce and usually self taught for nurses not part of peripherally inserted central catheter (PICC) teams.
- Lack of structured training and available ultrasound equipment has kept this desirable technique to among a few Registered Nurses (RNs) per facility.
- However, this is changing. Ultrasound equipment is getting smaller, less expensive and becoming more readily available.
- Introducing this skill into the hands of more nursing department will positively influence patient outcomes, reducing delay of care and peripheral iv insertion attempts.
The Need: Common Difficult Stick Causes1
| Diabetes | Obesity Increasing |
| Cancer | Hemophilia |
| Cardiovascular Conditions | Rheumatoid arthritis |
| End stage renal disease | Drug abuse |
| COPD | Crohns, ulcerative colitis, irritable bowel syndrome |
| Aging population | Dark pigmentation difficult to visualize vascular |
| Mastectomy | Hypotensive |
| Stroke | Multiple injuries |
| Contractures | History of multiple venous cannulations |
| Smoking | Immunodeficiency |
| Inactivity | Long periods of bedrest |
| Hematomas | Peripheral venous disease |
Example Program Content
As with any nursing procedure, a well written policy and competency in essential. Monitoring outcomes is also advised as this will alert the facility to any problems where additional training may be necessary and can also serve as an annual competency log. All of this program content (policy, competency, and outcomes log) is available upon request via email and attached as appendices. The author also suggests leaning on your vendors for assistance as they often support the sale of their products with the appropriate example documents.
Example Ultrasound Equipment

Although prices are coming down, portable ultrasound can be an expensive piece of equipment. Take care of it by always cleaning before and after use. Also using a sign-in/sign-out log book is helpful when others may be borrowing the equipment.
Tip: Wrap the cord around your arm helping prevent the probe from sliding off the bed when finished accessing the vessel.
Fig. 1 http://englishmotion.com.br/qtmove/includes/site-rite-vision-i2.jpg
Fig. 2 http://www.bardaccess.com/assets/images/products/ultrasound/siterite6_unit_hero.jpg
Fig. 3 http://65.36.201.165/instrumentpics/sonositeiLook.jpg
Ultrasound Technology1
- Ultrasound has a high frequency >20KHz, outside the range of human hearing.
- Interacts with tissues as it propagates and returns
- Reflections from blood are weak compared with those from solid tissues.
Ultrasound Equipment (tips)
- Always plug in power adapter
- Battery life is unpredictable
- Utilize a sign-in / sign-out log book
- Clean before and after use
- Please take careful care in handling equipment
- Very expensive... $5,000 - $25,000
- Replacement probe... $2,500+
- Do not drop it :)
- Avoid tilting the probe1
- Fig 1 “a” will produce the cleanest image
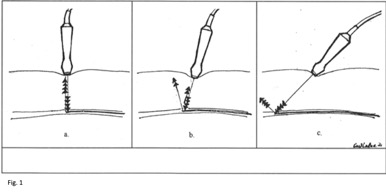
1. Ihnatsenka, International Journal of Shoulder Surgery, 2010, pg 7
Fig 1. http://vrassoc.com/Page24_Figure2.gif
Ultrasound – Maximize Your Image
- Depth
- The lumen should be large enough to be easily seen on the ultrasound screen.1
- Optional settings typically available
- gain, focus, etc
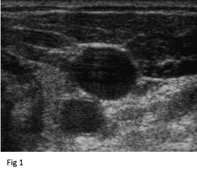
- Fluid filled vessels should appear (anechoic) black, void of echoes2
1. Goldstein, Israeli Journal of Emergency Medicine, 2006, pg 50
2. Ihnatsenka, International Journal of Shoulder Surgery, 2010, pg 7
Fig 1. http://www.ivteam.com/wp-content/uploads/2008/11/ultra.jpg
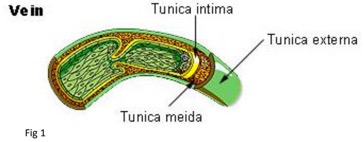
Vessel Selection: Vein Anatomy

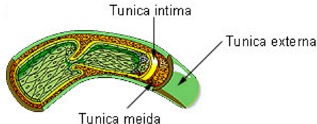
Fig 1 (left). http://images.tutorvista.com/content/transportation/illustration-of-normal-vein.jpeg
Fig 2 (right). http://www.daviddarling.info/images/vein.jpg
Vessel Selection: Arm Vein Anatomy
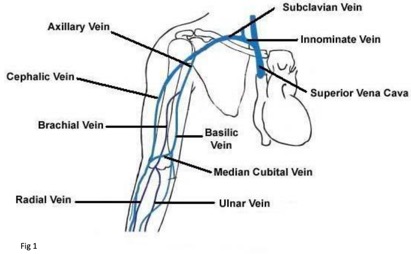
Fig 1. http://vascularultrasound.net/wp-content/uploads/2010/08/armveins2-copy.jpg
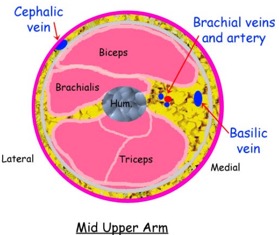
Source: http://www.ultrasoundpaedia.com/uploads/53003/ufiles/dvt-arm/dvt%20arm%20normal/upper-arm-vein-anatomy.jpg
Vessel Selection: Ultrasound View
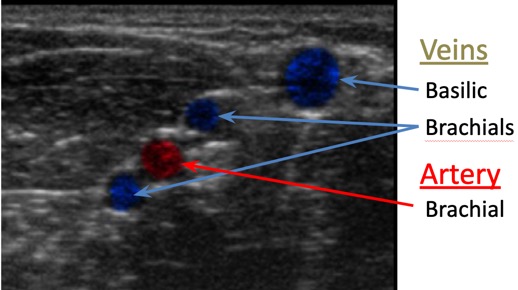
http://img.medscape.com/pi/emed/ckb/clinical_procedures/79926-104340-1433943-1464224.jpg
Vessel Selection: Typical Vein Sizes & Flow Rates
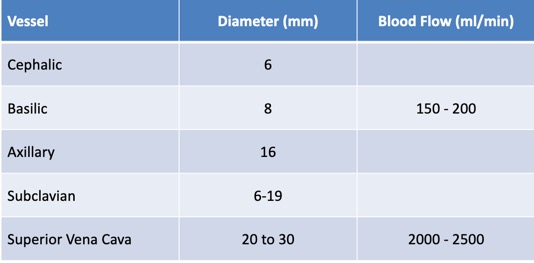
Reference: Ryder, Surgical Oncology Clinics of North America, 1995, p412.
Vessel Selection: “Rule of Thumb”
- Be patient
- Look for sites that will have the best possible success
- Use warm packs if extremities are cold to touch
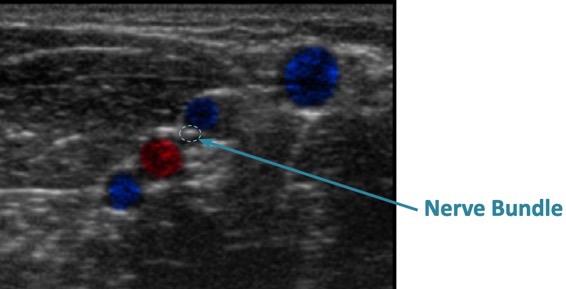
- Avoid areas of flexion1
- Use good judgment
- Evaluate and avoid sticking nerve bundles
Start where the vessels are known to be located in the antecubital area. Looking in a known location will help with gaining a familiarity of vessel appearance. Then scanning these vessels down the arm to a more appropriate site for a PIV is recommended. Scanning quickly takes a little practice and will become easy when coordination is developed. Another tip is to make deep depressions with the probe while moving side to side, as the vessels will "wink" at you making them easier to discern from their surroundings.
Reference: Policies and Procedures for Infusion Nursing, 4th ed. INS. P 58
-
Assess entire arm
-
Start distal and work up1
-
Ulnar, Radial, Cephalic
-
- Then..upper arm superficial
- Cephalic
- Avoid upper arm and forearm in patients with chronic kidney disease1
- Basilic, Brachial
1 Policies and Procedures for Infusion Nursing, 4th ed. INS. Pg 58,59.
Depth of the vein is important and the author cannot say this enough, "too deep of a vessel or a catheter that's too short may cause adverse outcomes." Ideally, vessels selected will be in the 0.5 cm to 1.25 cm range when using a catheter at least 1.75 in (4.5 cm).
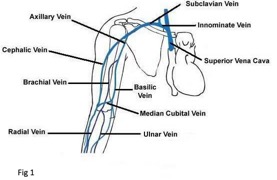
Fig 1. http://vascularultrasound.net/wp-content/uploads/2010/08/armveins2-copy.jpg
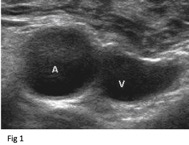
Vessel Selection: Vein vs Artery
The next step is differentiating vein from artery. Simple depression of the vessels by the probe will discover vein from artery. Veins will stay collapsed and arteries will pulsate, forcing their way open. Exceptions do exist of course. Some patients with very low blood pressures may not have enough arterial pressure to "pulsate" against the force of the probe. The best solution in that situation is to simply slowly let up the probe applying partial pressure until you see the pulsation begin.
Depress vessels to differentiate veins from arteries1
Vein will stay depressed.1
Arteries will “pulsate”1
Vein depth discussed later...
1. Meer, Medscape, 2011, pg 5
2. Goldstein, Israeli Journal of Emergency Medicine, 2006, pg 50
Fig 1. http://www.nysora.com/files/uploaded/techniques/ultrasound-guided_techniques/ultrasound-assisted_nerve_blocks/image6b_big.jpg
Selecting the Catheter
- Key Point 1 - While no industry standard exists on this, the author recommends the catheter length should be adequate to ensure that at least one-half of the catheter will reside in the vessel. This involves consideration of the angle of insertion and vein depth.
- Key Point 2 - The catheter should be easy to thread using only one hand, as the user’s other hand will be unavailable holding the probe.
- Key Point 3 - Catheter size (gauge) selection should reflect size of available vessel and types of therapy to minimize complication. Use the smallest diameter catheter needed in the largest available vein.1

- Example of typical catheter used for ultrasound guided PIV insertions
- 1.75 in | 45 mm (or longer)
- 20 gauge
- This will require adding tubing
- One handed insertion and threading should be possible with your choice of catheter
Fig 1. http://mtrhealth.com/wp-content/uploads/wpsc/product_images/B.%20Braun%20Introcan%20Safety%C2%AE%20IV%20Catheters.jpg
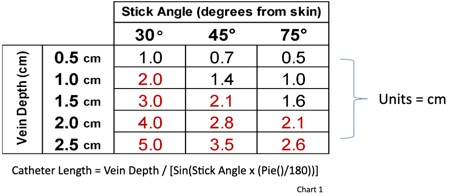
Vein Depth | Stick Angle | Catheter Length
Take notice of the catheter length needed to reach the vein (hypotenuse of the triangle). This can vary greatly depending on the angle of insertion chosen. Keeping this
angle in a range of 45 to 65 degrees will also help prevent two problems:
- Using a stick angle too small (close to the skin) will use up way too much of the catheter before reaching the vein, resulting in insufficient length of catheter left to dwell in the vein.
- Using a stick angle too steep (close to the probe) can often result in the catheter kinking at the hub as it is secured to the skin.
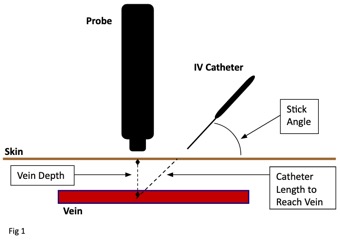
The author advises to stick at an approximate angle of 45 degrees or a little steeper. The use of a needle guide can also be a great tool to achieve a very accurate insertion
technique. This point not only prevents the aforementioned problems, but also makes seeing the tip of your needle much easier. "Steeper is easier."
- This chart represents the catheter lengths needed just to reach the vein.
- The length to reach the vein should not be more than one-half of your catheter length.
- Red = Areas of caution when using a 1.75in (4.5cm) catheter
Site Preparation
- Trace vein with probe to find a straight section of the vein 1
- Mark endpoints to visualize vein path 2
- Mark endpoints to visualize vein path and insertion area 1

1. Goldstein, Israeli Journal of Emergency Medicine, 2006, pg 50
Fig. 1 & 2: Image created by Kevin Arnold, RN, BSN. [email protected]
- Follow your facility protocol
- When using chorhexidine, friction is important, scrub the selected site about three inches in diameter for 30 sec and allow to dry1 NOTE: Do not blot or wipe on site to speed drying.
- Aseptic vs sterile technique is inconsistent in the literature. Minimizing contact of the needle with gel is intuitive but may difficult for novice users.2
- Apply sterile gel to the probe or above selected insertion site 3
- Alternate techniques: covers, gel caps, etc.
1. ChloraPrep One-Step FREPP Applicator, CareFusion, 2010
2. Goldstein, Ultrasound-Guided Peripheral Venous Access, 2006 pg 49
3. Meer, Ultrasonography Assisted Peripheral Line Placement, 2011, pg 6
Technique
- Clasp probe with a “C” grip close to the skin... holding the probe far from the end will allow too much movement1
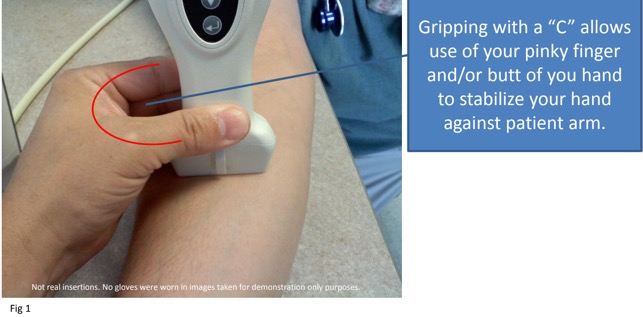
1. Ihnatsenka, International Journal of Shoulder Surgery, 2010, pg 7
Fig 1. Image created by Kevin Arnold, RN, BSN. [email protected]
- Stabilize your hand holding probe with one finger or wrist against patient’s arm.
- For users that place the machine on the same side of the bed, it is recommended to wrap the ultrasound cord around arm to prevent dropping probe.

- Keep ultrasound perpendicular to skin for a better image 1
- Use on-screen guide to align center. 2
1. Ihnatsenka, International Journal of Shoulder Surgery, 2010, pg 7
2. Goldstein, Israeli Journal of Emergency Medicine, 2006, pg 50
Fig 1. Image created by Kevin Arnold, RN, BSN. [email protected]
- AGAIN: Consider the concept of catheter length vs. angle of insertion. It is important to balance the two.
- Veins with a diameter of at least 0.4cm and a depth no greater than 1.5cm should yield better success.1
- Sticks will be easier with a higher angle of insertion, but this must be balanced with the catheter’s ability to bend.
- Avoid kinking the catheter.
- Center the vessel on the ultrasound probe1

- Use on-screen guide to measure depth of vein and direction. Each dot = 1⁄2 cm (on most machines).
- Threading: In general it is easier to visualize your needle if you stick in the 45 (to 65) degrees range from the skin.1 Then lower your angle to thread the catheter.2
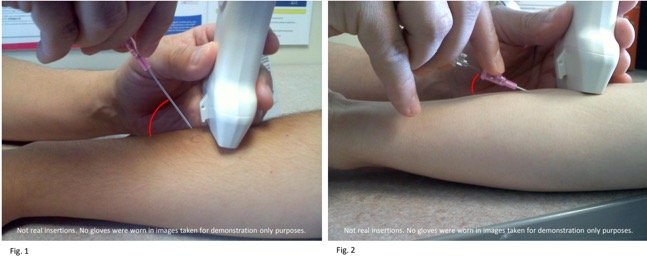
1. Meer, Ultrasonography Assisted Peripheral Line Placement, 2011, pg 7
2. BD Insyte Autogaurd IFU, http://www.bd.com/infusion/pdfs/d13348-4d.pdf, page 1
Fig. 1 & 2: Image created by Kevin Arnold, RN, BSN. [email protected]
- Scan probe to view needle tip by moving probe to and from insertion site. 1
- You may inadvertently stick through both sides of vein wall. If so, you may see and feel the vein wall “pop” into place when retracting the needle out of the deeper side of the vein wall.
- You should have excellent blood flow when tip is in the middle of the vein. 1
- After visualizing tip of needle in center of vein, it is okay to lessen the angle of the needle as you begin to thread the catheter.
1. Meer, Ultrasonography Assisted Peripheral Line Placement, 2011, pg 7
- Needle entering and visible in vein
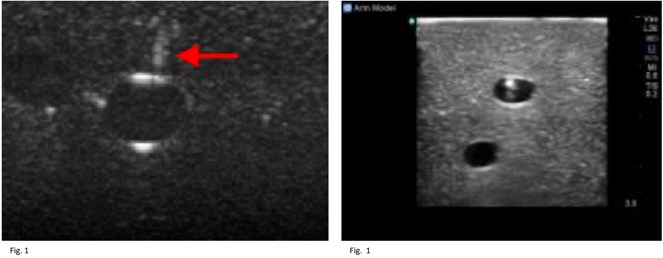
Fig. 1 http://img.medscape.com/pi/emed/ckb/clinical_procedures/79926-104340-1433943-1464756.jpg
Fig. 2 http://www.bluephantom.com/product_thumbs/t_basilic_vein_ultrasound_needle_cannulation_PICC_training.jpg
- Side View (Horizontal Plane)

Fig 1. http://www.bluephantom.com/product_thumbs/t_brachial_vein_ultrasound_needle_insertion_model.jpg
Documentation
- Follow facility protocol
- Typical: Document IV site location and preparation, gauge of catheter, number of attempts, and type of dressing in the medical record.
- Use of ultrasound for guidance should be included in note.
Potential Complications1
- Arterial puncture
- Adjacent nerve irritation
- Infection
- Infiltration
- Potential UE DVT
- Injury to vessel preventing arteriovenous fistulas sites for renal patients
1. Goldstein, Ultrasound-Guided Peripheral Venous Access, 2006 pg 51
Common Pitfalls
- Beware of threading in the “sidewall” of the vein.
- It is common to get some blood return after threading through part of the sidewall. It is very important to visualize the needle tip in the center of the vein opening.
- My needle is under the skin but I can’t see the tip?
- Make sure the needle is directly underneath the face of the transducer
- Move the transducer closer to the site of skin entry.
- You may be too deep. Look for movement below vein.
- I buried my needle and I still can’t reach the vein?
- Retract and advance at a steeper angle, but make sure to allow sufficient catheter length left for in the vein. Infiltration is likely if catheter is too short.
Summary Tips
- Keep your eyes on the screen...not the insertion area.
- Stick steeper...45 degrees is steeper than usual.
- Don’t hover over patient with needle...just stick quickly through skin and then use the screen to guide the needle into the vein.
- Use your wrist/finger to stabilize your probe hand...free handing the probe will allow too much movement.
- Use a “C” grip to hold the probe.
- Use minimal amount of gel. Too much gel creates a mess and difficulty.
- Avoid extreme steep angles as this may kink the catheter while securing to the skin.
Student/Patient Outcomes
- Barton and Danneck Average Stick Rate
- Traditional palpation method
- Mean num of IV attempts 2.18 1
- Poor patient satisfaction
- Hard Stick average
- ???
- zUltrasound PIV insertion using ultrasound
- My experience... as good as 1.10 = approx 90%
- Multiple studies report similar outcomes
1. Barton, Journal of Nusing Care Quality, 1998, pg 78
Typical Learning Curve
Average Sticks by New Ultrasound Users Post Check Off Insertions
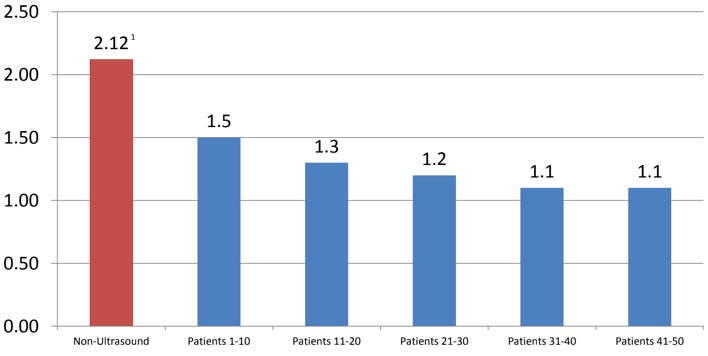
1. Barton, Journal of Nusing Care Quality, 1998, pg 78
Data generalized from course author’s teaching experience of typical outcomes.
Conclusion
Using ultrasound to place PIVs is becoming more prevalent beyond just the expert PICC nurse. It's pretty easy to see by those who have done it how implementing this new skill can lower the number of insertions per patient, save costs associated with those insertions, and reduce risks for infection and other adverse outcomes associated with repetitive vein trauma. Equipment is becoming more affordable, leaving facilities little reason not to pursue this superior practice.
Congratulations on completing the initial training towards improving your practice!
References
- Barton AJ;(1998) “Improving Patient Outcomes Through CQI: Vascular Access Planning” J NursCare Qual 13(2) 77-85
- BD Insyte Autogaurd IFU, http://www.bd.com/infusion/pdfs/d13348-4d.pdf, page 1
- Dychter SS: (March/April 2012) “Intravenous Therapy a Review of Complications and Economic Considerations of Peripheral Access, 35(2) 84-91
- Hadaway L. “The Iris Vascular Viewer” InfraRed Imaging Systems May 16, 2005. Pp. 1-4
- Ihnatsenka B, Boexaart A.: Ultrasound: Basic Understanding and Learning the Language, International Journal of Shoulder Surgery, 2010, pg 71-15
- Meer J M: Ultrasonography Assisted Peripheral Line Placement, Medscape, August 3, 2011, http://emedicine.medscape.com/article/1433943-overview#aw2aab6c10, pg 5
- Myers K., Clough A: Making Sense of Vascular Ultrasound – A Hands on Guide; 2004,Odder Arnold, United Kingdom, pg 1-341.
- Policies and Procedures for Infusion Nursing: Infusion Nurses Society, 4th Ed. 2011, pg 1-162
- Ryder MA; Peripheral Access Options, Surgical Oncology Clinics of North America; 4(3) pp 395-427
Appendix A: Example Policy
ULTRASOUND GUIDED PIV INSERTIONS & BLOOD DRAWS
INDICATIONS FOR USE:
a. Patients with difficult venous access may be candidates for US guided starts.
b. May utilize US for placement by health care workers with appropriate training.
PRECAUTIONS & KEY POINTS:
1. The deeper veins generally utilized for US guided starts are associated with a greater risk of complication from infiltration due to later recognition of infiltration and proximity of nerves and arteries.
2. The upper Brachial and Basilic veins may be considered if no other options are available.
3. Special consideration needs to be given to catheter selection based on the depth of the chosen target vessel. At least 1⁄2 of catheter length should reside in the vessel in final position.
4. Vein diameter should be 3x’s catheter diameter (with no tourniquet applied).
5. Local anesthetic may be utilized for US guided starts.
6. Special care must be taken to avoid possible infection during the procedure.
SECTION I: DIRECTIONS
1. Gather Equipment:
a. Portable US machine and gel.
b. IV supplies as per PIV protocol.
c. Appropriate IV safety catheter for selected target vessel.
d. Sterile US gel.
e. 2X2 gauze.
f. Local Anesthetic (optional).
2. Preparation for Insertion:
a. Prepare as per standard PIV procedure.
b. Position US machine for clear view with patients arm in comfortable position.
c. Open additional supplies; 2X2’s, sterile gel.
d. Draw up local anesthetic in labeled syringe and attach 25-30g needle (optional).
3. Site Selection:
a. Don PPE.
b. Apply non-Latex tourniquet snugly on upper arm.
c. Assess extremity for possible sites.
(1) Consider range of motion/restricted movement in selecting sites. Avoid joints (wrist/elbow) if possible.
(2) Consider purpose and duration of therapy. (e.g. phlebogenic solutions/drugs) Using non-sterile US gel, explore forearm for suitable target vessels. If no suitable veins are located, check other arm before proceeding to upper arm.
(3) If upper arm presents the only suitable vessels. Cephalic vein is best, followed by Basilic.
d. Vein diameter should be 3x’s catheter diameter (with no tourniquet applied)
e. Depress veins with U/S to differentiate veins from arteries. Veins will stay depressed. Arteries will “pulsate” due to pressure forcing blood through depression.
NOTE: Patients with low BP may not pulsate when depressed.
f. When appropriate target is selected, release tourniquet.
g. If no appropriate target vessel is identified discuss consideration of other type of access for the patient with the PICC RN and/or physician.
4. Catheter Selection:
a. Consider purpose and duration of therapy i.e. volume vs. multiple intermittent meds and/or isotonic fluids vs. phlebogenic drugs/solutions.
b. Catheter size selection should reflect size of available vessel and type of therapy to minimize/prevent complications and maintain adequate access.
NOTE: Phlebogenic drugs are best given through a small catheter in the largest available vessel.
c. Catheter length should be adequate to ensure that 1⁄2 of the catheter will reside in the lumen of the vessel. Be sure to take the angle of approach into consideration when determining vessel depth (scale available on US screen).
5. Site Preparation:
a. Using friction and approved skin antisepsis scrub the selected site about 3 inches in diameter for 30 sec and allow to dry.
NOTE: Do not blot or wipe on site to speed drying.
b. Reapply tourniquet.
c. Prep surface of transducer using Chloraprep sponge (once prepped, do not allow probe to contact non-prepped areas.)
d. Apply a small amount of sterile gel above selected insertion site
e. Visualize vein with transducer and administer local anesthetic as per protocol
6. Venipuncture/Insertion of Catheter/Blood Draw:
a. Reapply tourniquet.
b. Maintain sterility of catheter and integrity of prepared site during venipuncture. NOTE: Do not touch the site with your fingers once it has been prepped.
c. Using center mark of transducer aligned with vessel as guide, advance catheter into target vessel while watching/guiding tip progress with US. Adjust probe as needed, but do not overrun insertion site.
d. Once a blood return is visualized, lower angle of catheter and slide catheter off stylet into vessel to hub of catheter. Activate safety device. If blood draw, use appropriate device in place of catheter.
e. Set aside transducer, and release tourniquet.
f. Apply enough pressure above the end of the catheter to occlude it momentarily while attaching the extension set. Ensure good blood return. Slowly flush with NS, observing for swelling, then close clamp on the connector.
g. Wipe gel from around catheter using sterile 2X2’s.
h. Apply transparent dressing to cover insertion site and catheter hub.
i. Apply tape as needed to secure catheter/tubing. Do not place any tape under the dressing.
j. Write the date, type and gauge of catheter on the transparent dressing with a felt marker.
7. Documentation:
a. Document IV site location and preparation, gauge of catheter, number of attempts, type of dressing, and numbing agent, in the medical record. Use of Ultrasound for guidance should be included in note.
PATIENT EDUCATION:
Instruct patient this is an advanced way to see their veins. Pain of insertion is comparable to a regular PIV insertion. Anesthetic is available, but its sting is usually worse than the IV needle.
CLEANING PROCEDURES:
The ultrasound system probes should be cleaned between patient uses. To clean the ultrasound system/probe, 1. Turn off the system. 2. Dampen a nonabrasive cloth with warm water or rubbing alcohol. 3. Gently wipe the dampened cloth over exterior surfaces.
REFERENCES:
1. http://vascularultrasound.net/wp-content/uploads/2010/08/armveins2-copy.jpg
2. http://www.daviddarling.info/images/vein.jpg
3. http://vrassoc.com/Page24_Figure2.gif
4. http://www.bardaccess.com/assets/images/products/ultrasound/supporting/product-siterite-needles.jpg
5.http://www.ispub.com/ispub/ijms/volume_2_number_2_62/a_needle_guide_device_is_better_than_a_free_hand_technique_for_ultrasound_guided_cannulation_of_the_internal_jugular_vein_results_from_a_simulation_study/guide-fig3.jpg
6. http://img.medscape.com/pi/emed/ckb/clinical_procedures/79926-104340-1433943-1464224.jpg
7. http://www.sydneyendovascular.com.au/images/ultrasound3.jpg
8. http://www.ivteam.com/wp-content/uploads/2008/11/ultra.jpg
9. http://www.bluephantom.com/product_thumbs/t_basilic_vein_ultrasound_needle_cannulation_PICC_training.jpg
10. http://img.medscape.com/pi/emed/ckb/clinical_procedures/79926-104340-1433943-1464756.jpg
11. http://www.bluephantom.com/product_thumbs/t_brachial_vein_ultrasound_needle_insertion_model.jpg
12. Created by Kevin Arnold, PICC RN, BSN, [email protected]
13. Created by Kevin Arnold, PICC RN, BSN, [email protected]
Course Description
Course Objectives
Course Content
- Precision & Solution for the Hidden Veins
- Introduction
- The Need: Common Difficult Stick Causes1
- Example Program Content
- Example Ultrasound Equipment
- Ultrasound Technology1
- Ultrasound Equipment (tips)
- Ultrasound – Maximize Your Image
- Vessel Selection: Vein Anatomy
- Vessel Selection: Arm Vein Anatomy
- Vessel Selection: Ultrasound View
- Vessel Selection: Typical Vein Sizes & Flow Rates
- Vessel Selection: “Rule of Thumb”
- Vessel Selection: Vein vs Artery
- Selecting the Catheter
- Vein Depth | Stick Angle | Catheter Length
- Site Preparation
- Technique
- Documentation
- Potential Complications1
- Common Pitfalls
- Summary Tips
- Student/Patient Outcomes
- Typical Learning Curve
- Conclusion
- References
- Appendix A: Example Policy
Course Exam
Before you receive your certificate, you must complete the exam and achieve a score of % or higher. (You have unlimted attempts).
This exam is required by your state licensure.
Exam
Exam
We are required to delay the exam hours. Check back soon!
Exam
We are required to delay the exam until you have had time to view the course material. Please view the course first!
No Licenses on File
Please add a license to your account before you continue. Thank you!

